- MAIA Biotechnology is pioneering a breakthrough in cancer treatment, presenting a novel approach at the 2025 European Lung Cancer Congress in Paris.
- The focus is on Non-Small Cell Lung Cancer (NSCLC) with ateganosine as a key agent disrupting telomeric DNA, triggering cancer cell destruction.
- This method leverages both innate and adaptive immune responses, utilizing T-cells and the cGAS/STING pathway to combat tumor growth.
- Interleukin-6 (IL-6) emerges as a potential biomarker, offering personalized treatment strategies alongside checkpoint inhibitors.
- The highlight of the research will be presented by Dr. Tomasz Jankowski on March 28, 2025, marking a significant shift toward immunotherapy in cancer treatment.
- This development signals a paradigm shift in cancer care with targeted immunotherapies, enhancing outcomes and extending patient lives.
On the bustling stage of medical innovation, a promising development has emerged that could redefine the fight against cancer. MAIA Biotechnology, a pioneering force in immunotherapy, has announced a breakthrough study set to illuminate the halls of the European Lung Cancer Congress 2025 in Paris. Amidst the city’s iconic skyline, a novel approach to cancer treatment, tailored to combat the formidable Non-Small Cell Lung Cancer (NSCLC), sparks renewed hope.
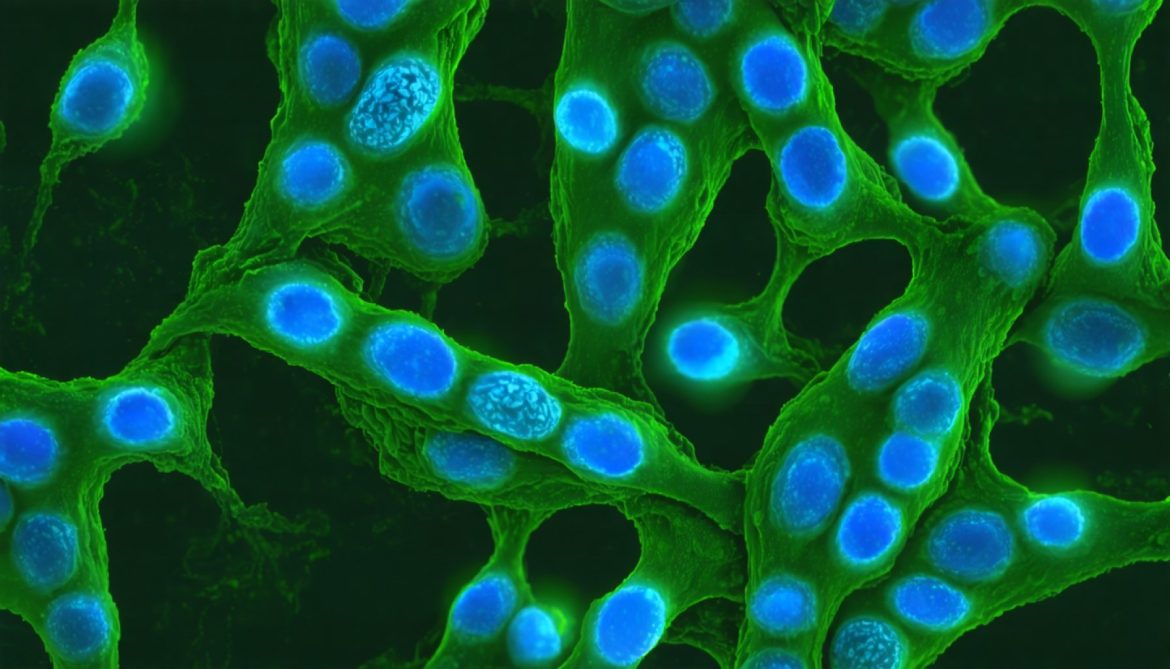
At the heart of this revelation is ateganosine (known by its research name, 6-thio-2’-deoxyguanosine), a trailblazing telomere-targeting agent. Imagine the telomeres—those protective tips of chromosomes—as the guardians of cellular longevity. However, in cancer cells, they become enablers of unchecked growth. Ateganosine emerges as the vigilant disruptor, intricately modifying telomeric DNA, sparking chaos within cancerous cells, and triggering their eventual demise.
The ingenious method employs the body’s own defenses, activating a dual assault with both innate and adaptive immune responses. Picture a battalion of T-cells and cGAS/STING pathway warriors, rallying against the cancerous tides, dismantling tumor strongholds in a strategic dance of science and biology. What follows is a spectacle of tumor regression—stubborn cells shrinking before an unwavering immune onslaught.
Yet, the breakthrough doesn’t end there. Enter Interleukin-6 (IL-6), a cytokine promising to play the unsung hero. As a potential predictive biomarker, IL-6 could tune the therapeutic symphony, providing a roadmap for personalized treatment strategies alongside checkpoint inhibitors. The symphony aims to transform resistance into remission, rewriting the stories of patients who have exhausted conventional therapies.
At the Congress, the findings take form—a vivid display led by Dr. Tomasz Jankowski. His team’s research is more than an academic endeavor; it’s the manifestation of a dream where science triumphs over mortality. The anticipation builds for March 28, 2025, at 12:00 p.m., as the world watches Paris not merely as a city of lights, but as a beacon for a new era in cancer medicine.
But what does this mean for a world yearning for progress against cancer’s relentless march? The implications are profound. This research is not just a whisper of hope; it is a clarion call for a paradigm shift in cancer treatment. MAIA’s vision ignites a path where targeted immunotherapies become the norm, reshaping outcomes and potentially extending lives.
In the fast-paced tide of discovery, one takeaway stands clear: the future of cancer treatment lies in the mastery of nature’s own arsenal, sculpting a future where the once-omnipotent foe may finally meet its match.
Revolutionary Advances in Cancer Treatment: Telomere-Targeting with Ateganosine
Unveiling the Potential of Ateganosine in Cancer Treatment
MAIA Biotechnology’s latest breakthrough in cancer treatment reveals a promising new approach at the upcoming European Lung Cancer Congress 2025. The trials involving ateganosine—a telomere-targeting agent—show potential to redefine how Non-Small Cell Lung Cancer (NSCLC) is tackled, fostering hope and excitement within the medical community.
Understanding the Mechanism of Ateganosine
Ateganosine, also known as 6-thio-2’-deoxyguanosine, ingeniously modifies the telomeric DNA in cancer cells. Telomeres, protective caps on chromosomes, usually degrade over time, leading to cell death. However, in cancer cells, telomerase enzyme reactivates these telomeres, allowing unchecked growth. Ateganosine disrupts this process, leading to cancer cell destruction from within.
Dual Immune Response Activation
The innovative treatment employs a dual-approach by leveraging both the innate and adaptive immune systems. T-cells and the cGAS/STING pathway work in tandem to aggressively target and destroy cancerous cells. This dual-action strategy may overcome hurdles faced in conventional therapies, offering renewed hope for improved patient outcomes.
Role of Interleukin-6 as a Biomarker
Interleukin-6 (IL-6) emerges as an essential component, assisting in predicting and personalizing treatment strategies. As a biomarker, IL-6 could pave the way for transforming patient resistance into remission, particularly when used alongside checkpoint inhibitors, customizing therapies to individual patient profiles.
How-To Include Ateganosine in Cancer Treatment
1. Evaluation: Patients must undergo comprehensive testing to determine eligibility for ateganosine-based treatment, focusing on the presence of NSCLC and telomerase activity.
2. Biomarker Analysis: Test levels of Interleukin-6 (IL-6) to predict therapy success and plan personalized treatment strategies.
3. Therapy Administration: Utilize ateganosine in conjunction with immune-checkpoint inhibitors to leverage dual immune response advantages.
4. Monitoring and Adjustment: Regular monitoring should be conducted to observe tumor response, with adjustments to therapy as necessary.
Real-World Implications and Industry Trends
The unveiling of MAIA’s study highlights the growing trend in personalized medicine and targeted immunotherapy treatments. As research progresses, it reinforces the movement towards therapies that integrate genetic and immune profiling, potentially setting a new standard in oncology treatments.
Anticipated Challenges and Considerations
While promising, this approach also has challenges:
– Patient Selection: Not all cancers exhibit high telomerase activity; thus, careful selection of eligible patients is crucial.
– Side Effects: As with any new treatment, managing potential side effects and reactions remains vital.
– Cost and Accessibility: Scaling the production of ateganosine and ensuring patient access are logistical and financial hurdles that need addressing.
Pros & Cons Overview
Pros:
– Potentially effective against aggressive NSCLC
– Personalized treatment approaches
– Activation of dual immune responses
Cons:
– Still under study; long-term effects unknown
– May not be suitable for all cancer types
– Complex treatment administration
Final Insights and Recommendations
For practitioners:
– Stay updated on the latest research findings and clinical trial results related to ateganosine.
– Consider integrating biomarker analysis into standard cancer treatment protocols to optimize therapy outcomes.
For patients:
– Consult with oncologists about emerging therapies and eligibility for personalized treatment options.
– Participate in clinical trials to access cutting-edge treatment.
For more on pioneering cancer therapies and advancements, visit American Cancer Society and National Cancer Institute. These leading institutions offer comprehensive resources on cancer research and treatment options.